Prolotherapy 101: What is a Sugar Water Injection
What is this “sugar water” injection that everyone is talking about? And how can it help with healing and pain?
Prolotherapy has been around since the 1930s when Dr. Earl Gedney, an osteopathic physician, developed a technique to heal his own injured ligaments when he hyperextended his thumb on closing surgical doors.1 However, in the 1950s Dr. George Hackett named the technique, prolotherapy, after observing a growth of new tissue at the junction of ligament and bone following an injection of a proliferant solution to the area.2
The theory behind prolotherapy is that when ligaments and tendons are loose or injured, they no longer provide stability to the joints they surround. The body then compensates by using the muscles around the injured region to provide the stabilization, resulting in muscle spasm.
Ligaments and tendons have relatively poor blood supply; however, they are richly innervated with pain fibers.2 When ligaments and tendons get injured, they never completely heal to their pre-injured state, and the recovery is usually prolonged. Chronic pain can ensue when there is lack of healing of these tendons and ligaments.
Understanding Sugar Water Injections
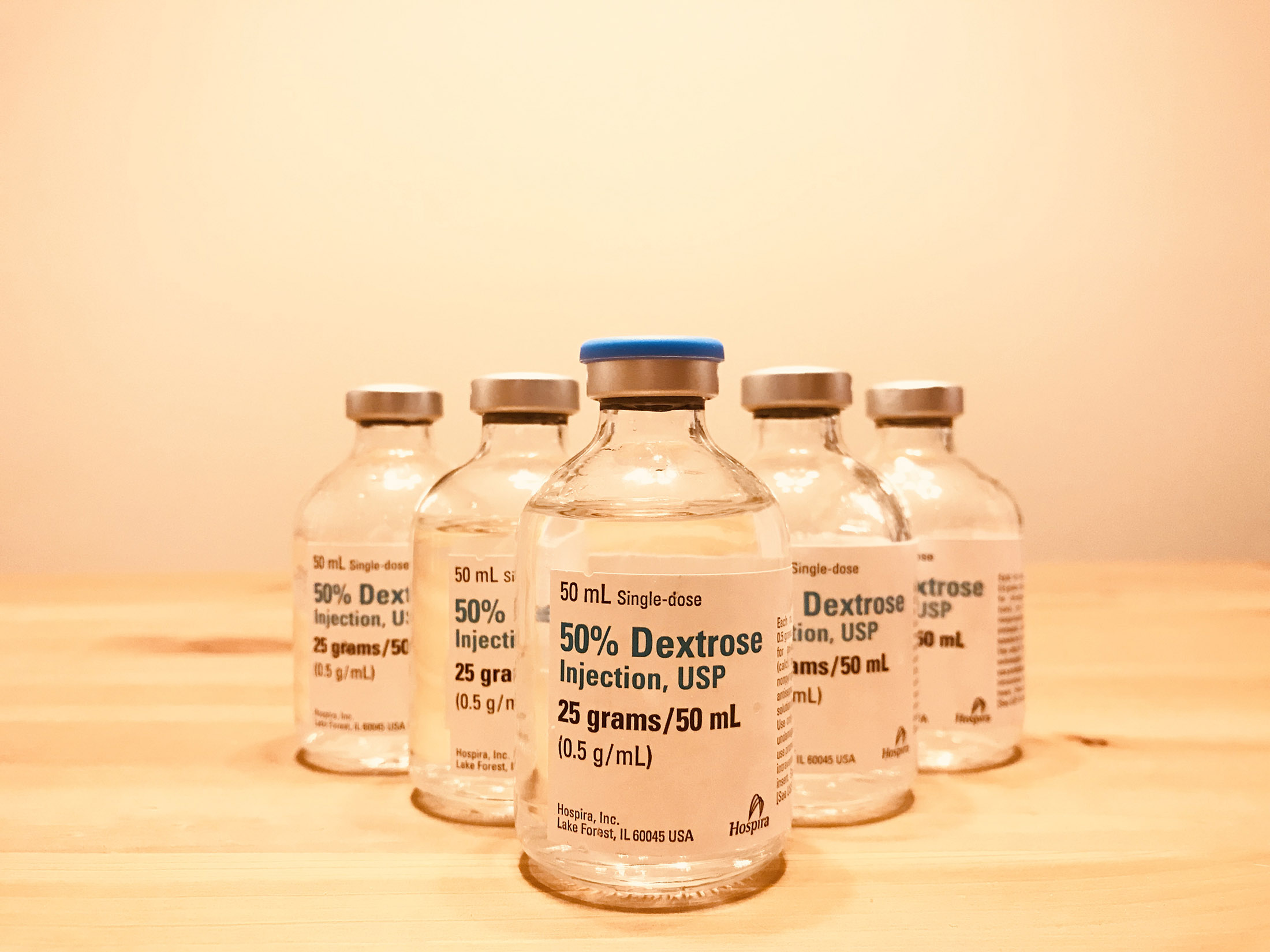
Prolotherapy involves injecting an irritant solution, usually a combination of dextrose (sugar), saline (salt), and a local anesthetic such as lidocaine. However, there are other solutions that can be used such as concentrated 23.4% saline and platelet-rich-plasma (PRP), to name a couple.
This irritant solution is injected into ligaments and tendons where they attach to bone (also known as entheses) to restimulate the body’s natural injury-healing process. This occurs over a period of 6-8 weeks. The new connective tissue that is laid down will then mature and become stronger over the next 12-24 months,3 which should provide more stability and decrease pain stemming from these structures.
What Are They Used to Treat?
There have been animal studies4,5,6 that have shown an increase in ligament and tendon thickness after prolotherapy injections compared to controls. Studies have also shown prolotherapy may be effective in treating chronic pain by modulating Substance P, a pain-producing molecule found in sensory nerve fibers, thereby reducing the transmission of pain signals. A,B This may explain the rapid pain reduction some patients experience following prolotherapy injection. C
There are multiple publications on prolotherapy, demonstrating its benefit in treating chronic musculoskeletal and sports injuries associated with unhealed ligament and tendon damage, which if left untreated can lead to the sequelae of unstable joints, osteoarthritis, and eventually pain.7,8,9
Chronic tendinopathy due to repetitive/overuse injury can be treated with prolotherapy with studies showing benefits in pain and function in individuals with tennis elbow.10,11 A review published in February 2019 looked at corticosteroids, prolotherapy, and PRP for treatment of rotator cuff tendinopathy, and concluded that prolotherapy and PRP provided significant pain reduction and improvement in shoulder function in the long term (more than 24 weeks), compared to corticosteroid injections, which only provided short-term relief of pain and improved function.12
However, prolotherapy has also been proven to provide equally good short-term (3 and 12-weeks) pain reduction and functional improvement when compared to corticosteroid injection for rotator cuff-related shoulder pain. D Prolotherapy has also been shown to be superior to exercise alone for improvements in pain and function related to knee osteoarthritis.13
A recent meta-analysis, including over 300 patients with knee osteoarthritis, found prolotherapy significantly improved knee pain and function when compared to placebo injection or exercise alone. E In addition to these studies, prolotherapy has also been shown to significantly improve pain long term at 15 months when compared to corticosteroid injections in patients with sacroiliac joint pain14 and neck pain studied 1 to 39 months post-treatment.15
When Do We Recommend a Sugar Water Injection
Prolotherapy can be a better option for pain and recovery than the usually accepted treatments such as corticosteroids (e.g., cortisone injections) and non-steroidal anti-inflammatory (NSAIDs) medications. This is important to note because studies have shown that corticosteroid injections are harmful to tendons, ligaments, and joint cartilage.16
In addition, NSAIDs have been shown to impair healing at the entheses17 and damaged cartilage.18,19 Also, NSAIDs appear to significantly elevate cardiovascular risk. In contrast, prolotherapy has been demonstrated to be a safe alternative therapy for a variety of painful conditions. 7,F,
How Many Injections Do You Need?
Typically, one treatment session of prolotherapy will not provide a complete resolution of pain. The number of sessions needed for treatment depends on the injury’s extent and the individual’s overall health. If you have musculoskeletal pain that does not seem to heal and are uninterested in surgery, prolotherapy may be a good treatment option for you. To learn more about these injections and see if you are a good candidate, please call our office and make an appointment.
Please note that there are different providers (DO, MD, and NMD) that perform prolotherapy in Arizona, and we recommend that you do your research on the credentials and training of these providers (such as their educational backgrounds, what conferences they have attended to learn prolotherapy techniques, and how they perform their prolotherapy).
Visit Us at Desert Spine & Sports
Here at Desert Spine and Sports Physicians, Dr. Tima Le performs these injections under ultrasound guidance, fluoroscopic guidance, and palpation guidance. She attends yearly conferences on prolotherapy and regenerative medicine to keep up and improve her skills as a prolotherapist.
References:
- Gedney EH. 1937, June. Hypermobile joint: a preliminary report. Osteopath Prof. 4(9):30-31.
- Hackett GS, Henderson DG. Joint stabilization: an experimental, histologic study with comments on the clinical application in ligament proliferation. Amer J Surg. 1955; 89:968-973.
- https://www.ncbi.nlm.nih.gov/books/NBK3938/
- Liu YK, Tipton CM, Matthes RD, Bedford TG, Maynard JA, Walmer HC. An in-situ study of the influence of a sclerosing solution in rabbit medial collateral ligaments and its junction strength. Connect Tissue Res. 1983; 11:95–102
- Maynard JA, Pedrini VA, Pedrini-Mille A, Romanus B, Ohlerking F. Morphological and biochemical effects of sodium morrhuate on tendons. J Orthop Res. 1985; 3:236–248.
- Jensen, KT, et al. Response of knee ligaments to prolotherapy in a rat injury model. American Orthopaedic Society for Sports Medicine; 2008.
- Rabago D, Best TM, Bearnsley M, et al. A systematic review of prolotherapy for chronic musculoskeletal pain. Clin J Sport Med 2005; 15:376-380.
- Hackett GS, Hemwall GA, Montgomery GA. Ligament and Tendon Relaxation Treated by Prolotherapy, 5th ed. Oak Park, IL, Gustav A. Hemwall; 1993
- Distel LM, Best TM. Prolotherapy: a clinical review of its role in treating chronic musculoskeletal pain. PMR. 2011; 3(6 suppl 1):S78–81.
- Rabago D, Best TM, et al. A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med 2009; 43:471–481.
- Rabago D, Lee KS, Ryan M, et al. Hypertonic dextrose and morrhuate sodium injections (prolotherapy) for lateral epicondylosis (tennis elbow): results of a single blind, pilot-level, randomized controlled trial. Am J Phys Med Rehabil 2013; 92:587–596.
- Lin MT, Chiang CF, et al. Comparative Effectiveness of Injection Therapies in Rotator Cuff Tendinopathy: A Systemic Review, Pairwise and Network Meta-analysis of Randomized Controlled Trials. Arch Phys Med Rehabil. 2019 Feb; 100(2):336–349.
- Sit RW, Chung VCH, Reeves KD, et al. Hypertonic dextrose injections (prolotherapy) in the treatment of symptomatic knee osteoarthritis: A systematic review and meta-analysis [published correction appears in Sci Rep. 2017 Apr 07; 7:45879]. Sci Rep. 2016; 6:25247. Published 2016 May 5. doi:10.1038/srep25247
- Kim WM, Lee HG, et al. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010; 16(12):1285–1290.
- Ross A. Hauser, Danielle Steilen, Karina Gordin. The Biology of Prolotherapy and Its Application in Clinical Cervical Spine Instability and Chronic Neck Pain: A Retrospective Study. European Journal of Preventive Medicine. Vol. 3, No. 4, 2015, pp. 85-102. doi: 10.11648/j.ejpm.20150304.11
- Hauser RA. The deterioration of articular cartilage in osteoarthritis by corticosteroid injections. Journal of Prolotherapy. 2009; 2:107–123.
- Su, Bailey, and J Patrick O’Connor. “NSAID therapy effects on healing of bone, tendon, and the enthesis.” Journal of applied physiology (Bethesda, Md.: 1985) vol. 115,6 (2013): 892-9. doi:10.1152/japplphysiol.00053.2013
- Kalbhen DA. The inhibitory effects of steroidal and non-steroidal antirheumatic drugs on articular cartilage of osteoarthrosis and its counteraction by a biological GAG-peptide complex (Rumalon). Z Rheumatol. 1982;41(5):202–211.
- Chang JK, Wu SC, Wang GJ, Ho ML. Effects of non-steroidal anti-inflammatory drugs on cell proliferation and death in cultured epiphyseal-articular chondrocytes of fetal rats. Toxicology. 2006; 228(2–3):111–123.
- Han DS, Lee CH, Shieh YD, Chang CT, Li MH, Chu YC, Wang JL, Chang KV, Lin SH, Chen CC. A role for substance P and acid-sensing ion channel 1a in prolotherapy with dextrose-mediated analgesia in a mouse model of chronic muscle pain. Pain. 2021 Aug 9. doi: 10.1097/j.pain.0000000000002440. Epub ahead of print. PMID: 34382604.
- Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology. 2018 Aug;129(2):343-366. doi: 10.1097/ALN.0000000000002130. PMID: 29462012; PMCID: PMC6051899.
- Maniquis-Smigel L, Dean Reeves K, Jeffrey Rosen H, Lyftogt J, Graham-Coleman C, Cheng AL, Rabago D. Short Term Analgesic Effects of 5% Dextrose Epidural Injections for Chronic Low Back Pain: A Randomized Controlled Trial. Anesth Pain Med. 2016 Dec 6;7(1):e42550. doi: 10.5812/aapm.42550. PMID: 28920043; PMCID: PMC5554430.
- Nasiri A, Mohamadi Jahromi LS, Vafaei MA, Parvin R, Fakheri MS, Sadeghi S. Comparison of the Effectiveness of Ultrasound-Guided Prolotherapy in Supraspinatus Tendon with Ultrasound-Guided Corticosteroid Injection of Subacromial Subdeltoid Bursa in Rotator Cuff-Related Shoulder Pain: A Clinical Trial Study. Adv Biomed Res. 2021 Mar 30;10:12. doi: 10.4103/abr.abr_181_20. PMID: 34195156; PMCID: PMC8204815.
- Wang J, Liang J, Yao J, Song HX, Yang XT, Wu FC, Ye Y, Li JH, Wu T. Meta-analysis of clinical trials focusing on hypertonic dextrose prolotherapy (HDP) for knee osteoarthritis. Aging Clin Exp Res. 2021 Aug 27. doi: 10.1007/s40520-021-01963-3. Epub ahead of print. PMID: 34449061.
- Hauser RA, Lackner JB, Steilen-Matias D, Harris DK. A Systematic Review of Dextrose Prolotherapy for Chronic Musculoskeletal Pain. Clin Med Insights Arthritis Musculoskelet Disord. 2016 Jul 7;9:139-59. doi: 10.4137/CMAMD.S39160. PMID: 27429562; PMCID: PMC4938120.
